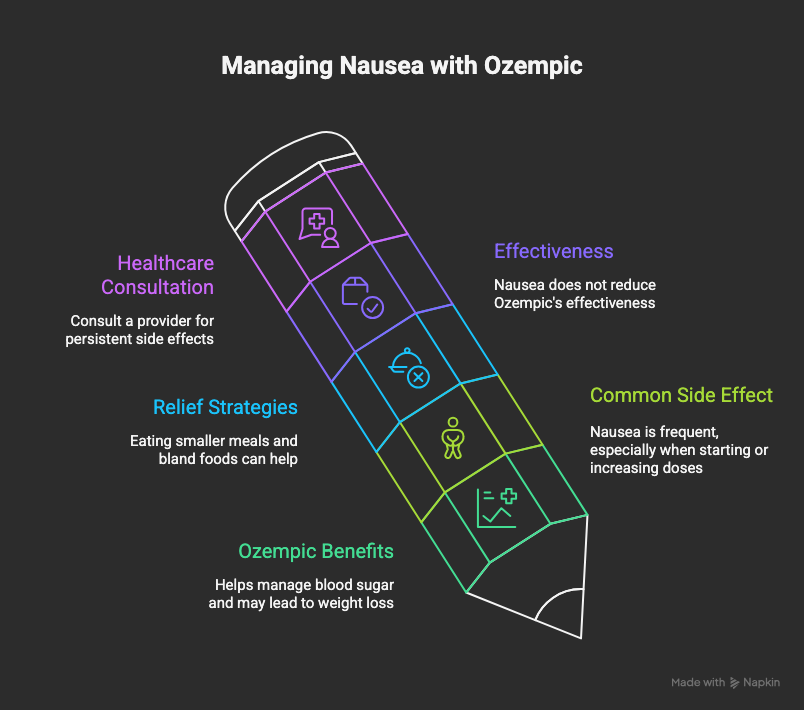
Key Highlights
- Ozempic is a medication for type 2 diabetes that can help manage blood sugar levels and may lead to weight loss.
- Nausea is one of the most common side effects of Ozempic, especially when starting the medication or increasing your dose.
- You can find nausea relief by eating smaller, more frequent meals and choosing bland, low-fat foods.
- While nausea can be challenging, it does not typically reduce the effectiveness of Ozempic for blood sugar control or weight management.
- Always consult your healthcare provider about any persistent side effects for professional guidance and possible dose adjustments.
Introduction
Starting Ozempic treatment can be an important step in managing your blood sugar and supporting your health goals. However, a common hurdle many people face is nausea. This uncomfortable side effect can impact your daily life, but the good news is that it’s often manageable. This article will walk you through why nausea happens with Ozempic and provide practical tips and strategies to help you find relief and continue your treatment with greater comfort.
Understanding Ozempic and Its Role in Blood Sugar Management
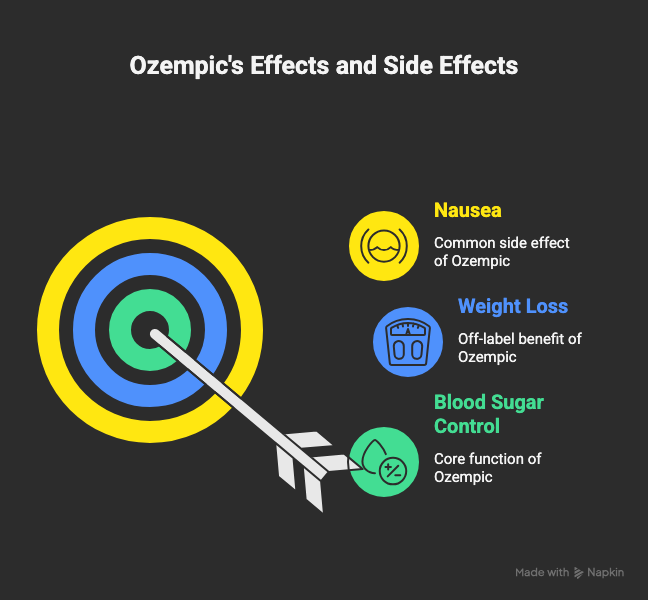
Ozempic is an injectable medication primarily used to improve blood sugar control in adults with type 2 diabetes. It is also sometimes prescribed off-label for weight management. By mimicking a natural hormone, it helps regulate blood sugar and can lead to weight loss, making it a valuable tool among diabetes medications.
However, the way Ozempic works in your body can also lead to certain side effects. Understanding this mechanism is the first step to learning why you might feel nauseous and how to manage it as you adjust to your Ozempic dose.
Nausea as a Side Effect of Ozempic
If you’re feeling nauseous after starting Ozempic, you are not alone. Nausea is the single most commonly reported side effect of Ozempic. This feeling is a direct result of the medication’s impact on your digestive system, and it often appears when you first begin treatment or increase your dose.
Understanding why this happens is key to finding effective nausea relief. Let’s look closer at the mechanisms behind this common complaint and how often people experience it.
How Frequently Does Nausea Occur with Ozempic Use?
Nausea is one of the most common side effects of Ozempic, but how often does it really happen? Clinical trials provide clear data on its prevalence. In these studies, the frequency of nausea was directly related to the dosage of the medication.
For example, about 15% of participants taking a 0.5 mg dose of Ozempic reported nausea, while that number increased to 20% for those on a 1 mg dose. This shows that as the dose goes up, the likelihood of experiencing gastrointestinal side effects also tends to increase.
Here is a look at the frequency of common adverse effects seen in clinical trials:
|
Side Effect |
Frequency (0.5 mg dose) |
Frequency (1 mg dose) |
|---|---|---|
|
Nausea |
15% |
20% |
|
Vomiting |
Less than 10% |
Less than 10% |
|
Diarrhea |
~8% |
~8% |
|
Constipation |
~5% |
~5% |
Timeline of Nausea After Starting Ozempic
When you begin taking Ozempic, you might wonder when nausea will start and how long it will stick around. Typically, digestive side effects like nausea appear shortly after starting Ozempic or after your doctor increases your dose.
The good news is that for many people, this is a temporary phase. As your body gets used to the medication, the nausea often subsides. The following sections will provide a more detailed timeline and explain what factors might influence how long these symptoms last.
management to minimize discomfort.
Adjusting Ozempic Dosage Safely with Your Doctor
If nausea is a persistent problem, one of the most effective medical strategies is to adjust your Ozempic dose. Your health care provider might suggest temporarily returning to a lower dose that you tolerated well. This can give your body more time to adapt before trying to increase the dose of Ozempic again.
Another option is a slower titration schedule. Instead of increasing your dose every few weeks, your doctor might recommend a more gradual increase over a longer period. This gentle approach can significantly reduce the intensity of side effects.
It is crucial that you never adjust your dose on your own. Always work with your health care provider to create a plan that is safe and effective. They will help you find the right balance to manage your blood sugar while keeping side effects to a minimum.
Conclusion
Navigating the journey with Ozempic can sometimes be challenging, especially when nausea becomes a side effect. However, understanding how Ozempic works and recognizing that nausea is a common experience can help ease your concerns. By implementing lifestyle strategies and practical tips discussed throughout this blog, you can significantly minimize discomfort. Remember, it’s always important to consult your healthcare provider for personalized advice and to adjust dosages if necessary. Taking care of your health is vital, and with the right approach, you can enjoy the benefits of Ozempic while managing any unpleasant symptoms. If you have further questions or need guidance, don’t hesitate to reach out for support!
Frequently Asked Questions
Should I Be Concerned if My Nausea Doesn’t Improve?
Yes, if your nausea is severe, persistent, or accompanied by other serious side effects like severe abdominal pain, you should seek medical attention. Continuous nausea can impact your nutrition and quality of life, so it’s important to get medical advice to rule out more serious issues and find a solution.
Does Nausea Affect My Results with Ozempic?
While nausea is an uncomfortable side effect, it does not reduce the effectiveness of the medication. Ozempic will continue to work on your blood sugar levels and support weight loss even if you feel nauseous. However, managing this symptom is important for your overall well-being and ability to stick with the treatment.
Are There Any Long-Term Risks if I Have Ongoing Nausea on Ozempic?
Ongoing nausea itself is not typically a long-term risk, but it could lead to poor nutrition or dehydration if it prevents you from eating and drinking properly. It’s crucial to discuss persistent adverse effects with your health care provider to ensure there isn’t an underlying serious issue and to get proper medical advice.