
Key Highlights
Here are the key points to remember about Ozempic and its effect on your digestive health:
- Ozempic constipation is a common side effect because the medication slows down your digestive system.
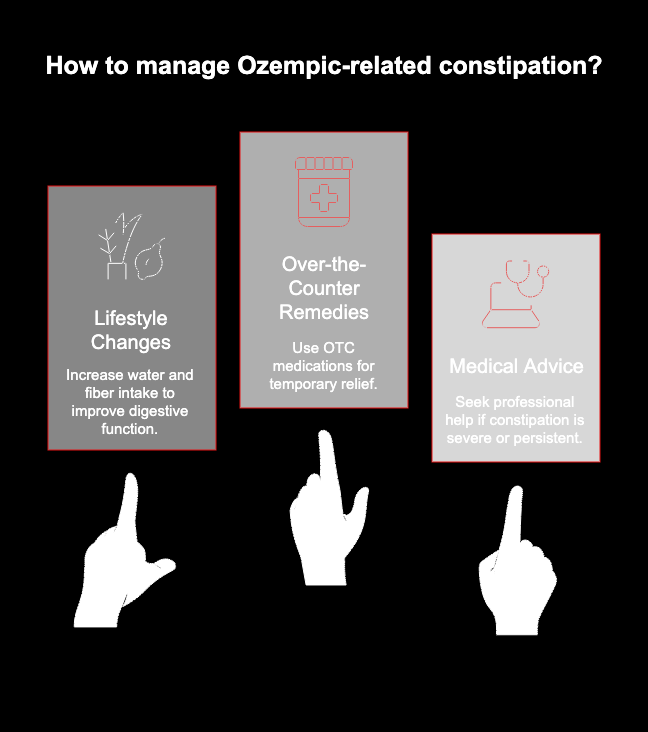
- This side effect can often be managed with simple lifestyle changes, including increased water and fiber intake.
- Treatment options for constipation relief range from diet adjustments and exercise to over-the-counter remedies.
- Higher doses of Ozempic may increase the likelihood of experiencing gastrointestinal side effects.
- It is important to seek medical advice if constipation is severe or does not improve with home care.
Introduction
Ozempic is a widely used prescription medication effective for managing type 2 diabetes and, in some cases, for weight loss. While it offers significant benefits, it’s also associated with certain side effects, particularly those affecting the digestive system. One of the most frequently discussed issues is Ozempic constipation. This discomfort can be frustrating, but understanding why it happens is the first step toward finding relief. This guide will walk you through the causes of constipation with Ozempic and what you can do about it.
Key Takeaways About Ozempic and Constipation
Constipation is a common side effect when you begin Ozempic treatment. The medication works by slowing down your digestive tract, which is great for feeling full longer but can lead to less frequent bowel movements. This change can impact your quality of life, but it’s often a manageable issue.
Fortunately, there are many effective strategies to counteract this side effect. From simple lifestyle adjustments to over-the-counter aids, you can take steps to get your system back on track.

How Common Is Constipation with Ozempic?
The frequency of constipation can vary depending on why you are taking Ozempic. During clinical trials focused on type 2 diabetes, a relatively small percentage of participants reported this side effect. However, research suggests it is more prevalent among those using the medication for weight management.
Interestingly, the dose you take might also play a role. Some data indicates that higher doses of semaglutide, the active ingredient in Ozempic, are linked to a greater chance of experiencing gastrointestinal adverse events like constipation. As your body adjusts, these side effects may lessen.
Here’s a quick breakdown of its prevalence based on use:
|
Condition Treated |
Percentage of Users Experiencing Constipation |
|---|---|
|
Type 2 Diabetes |
3-5% |
|
Obesity (Weight Loss) |
Approximately 24% |
Understanding Ozempic: What It Is and How It Works
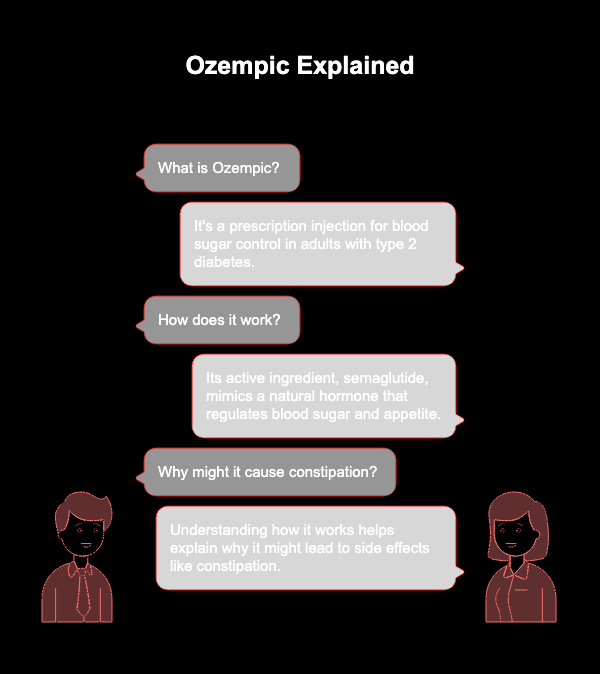
Ozempic is a prescription medication administered via injection, primarily used for blood sugar control in adults with type 2 diabetes. Its active ingredient, semaglutide, belongs to a class of drugs known as GLP-1 receptor agonists. These drugs mimic a natural hormone in your body that helps regulate blood sugar and appetite.
By understanding how this medication functions, you can better grasp why it might lead to side effects like constipation. Below, we’ll explore its role in weight management and its direct effects on your digestive system.
How Ozempic Affects the Digestive System
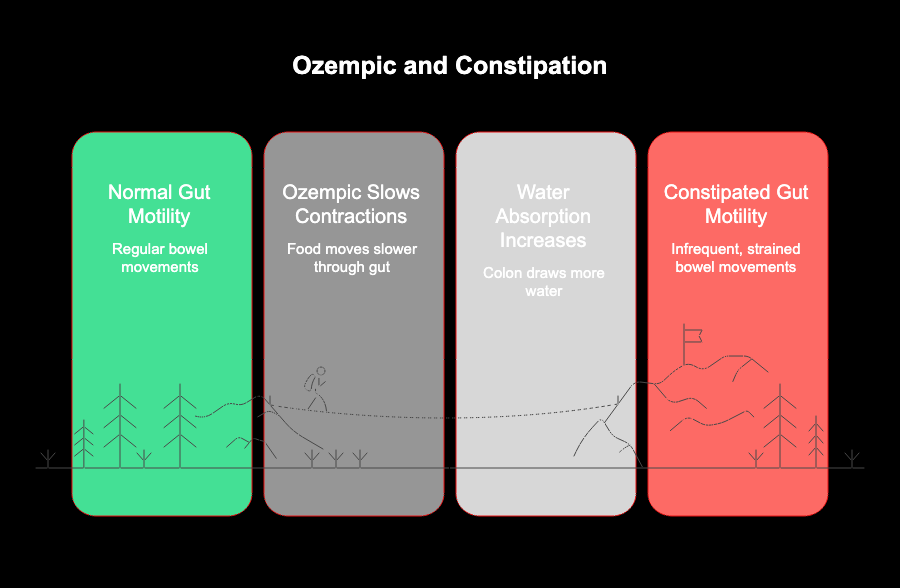
The primary way Ozempic impacts your digestive system is by slowing down gastric emptying. This means food stays in your stomach for a longer time before moving into the intestines. While this helps you feel satisfied and control your appetite, it also slows down the entire digestive process.
This change in gut motility is a key reason behind the common side effects of the medication. When the movement of food and waste through your system is delayed, it can lead to issues like nausea, bloating, and constipation.
Your body is essentially taking more time to process what you eat. This slowdown gives your intestines more opportunity to absorb water from the stool, which can make it harder and more difficult to pass, leading to constipation.
Changes in Gut Motility and Digestion
The term “gut motility” refers to the muscular contractions that move food through your digestive tract. Ozempic, through its active ingredient semaglutide, directly reduces the speed of these contractions. This is a deliberate effect designed to make you feel fuller longer.
However, this slowdown has a ripple effect. As waste material spends more time in your colon, your body continues to draw water from it. This process can leave your stool hard, dry, and difficult to pass, resulting in an infrequent or strained bowel movement.
This change in digestive speed is a central point to grasp. While it’s a key part of how the medication helps with weight loss and blood sugar, it’s also the direct cause of constipation for many users, as confirmed in clinical trials.
Interactions with the Gastrointestinal Tract
The gastrointestinal side effects of Ozempic go beyond just slowed digestion. Because you feel fuller, you might naturally start to eat and drink less. A lower intake of food can mean you’re not getting enough fiber, a crucial nutrient for maintaining regular bowel movements. Similarly, drinking less water can contribute to dehydration, which further hardens stool.
These factors combine to create a perfect storm for constipation. You might experience common symptoms like bloating and mild stomach pain.
It’s important to differentiate this discomfort from severe abdominal pain. While mild symptoms are expected, intense pain could signal a more serious issue. Managing your diet and fluid intake is key to mitigating these gastrointestinal interactions while still benefiting from better blood sugar levels.
Signs to Watch For in Bowel Movements
Changes in your bowel habits are the first indicator of constipation. It’s not just about how often you go; the consistency and effort involved are also important clues. Pay attention to how you feel during and after using the restroom.
If you’re dealing with constipation, you might notice that your trips to the bathroom have become more difficult. This can be accompanied by abdominal pain or a persistent feeling of fullness or bloating, even when you haven’t eaten much.
Here are some specific signs that point to constipation:
- Having fewer than three bowel movements a week.
- Stools that are hard, dry, or lumpy.
- Straining or pain during a bowel movement.
- A feeling that you haven’t completely emptied your bowels.
Lifestyle Adjustments to Support Regularity
Making small adjustments to your daily routine can significantly improve regularity. One of the most important lifestyle changes is to increase your physical activity. Exercise helps stimulate the natural contractions of your intestinal muscles, promoting healthier bowel movements. Even a daily walk can help.
Another key factor is hydration. When your body is dehydrated, it pulls more water from your stool, making it harder. Drinking plenty of water throughout the day is essential for keeping your stool soft and easy to pass.
Consider these simple but effective habits:
- Boost your fluid intake: Aim for around 9 cups of water daily for women and 13 for men.
- Get moving: Incorporate at least 30 minutes of regular physical activity into your day.
- Increase fiber slowly: Gradually add more fiber to your diet to allow your digestive system to adjust without causing more bloating.
Treatment Options for Ozempic-Related Constipation
If lifestyle changes aren’t providing enough constipation relief, other treatment options are available. These range from natural home remedies to over-the-counter medications that can offer more immediate results. It’s important to know which solutions are safe for short-term use and when it’s necessary to seek medical advice.
Below, we’ll cover some gentle home care strategies as well as common over-the-counter remedies. Understanding these choices will empower you to manage your symptoms effectively.
Conclusion
Understanding the relationship between Ozempic and constipation is crucial for anyone using this medication. While it can be an effective tool for weight management, its effects on the digestive system can lead to uncomfortable symptoms. By recognizing the signs of constipation and implementing practical lifestyle adjustments, you can significantly alleviate discomfort. Remember that good hydration, dietary choices, and, when necessary, treatment options can help maintain regularity. If you’re experiencing persistent issues, don’t hesitate to reach out to your healthcare provider. Taking proactive steps ensures that you can enjoy the benefits of Ozempic while minimizing any digestive concerns. For personalized advice, feel free to schedule a free consultation with our experts!
Frequently Asked Questions
How long does constipation from Ozempic last?
The duration of constipation from Ozempic varies. In some clinical trials, the issue resolved for many participants by the seventh week. However, for others, it may last longer. Your body’s adjustment period, Ozempic dosage, and lifestyle habits all play a role in how long this adverse event affects your digestive health.
Can drinking more water help with constipation caused by Ozempic?
Yes, absolutely. Drinking plenty of water is one of the most effective ways to find constipation relief. Increased fluid intake helps soften your stool, making it easier to pass through the digestive tract. This is especially important since Ozempic slows digestion, giving your body more time to absorb water from your bowels.
When should I call my doctor about constipation on Ozempic?
You should seek medical advice if your constipation lasts more than two weeks despite trying home remedies. It’s also crucial to seek immediate medical attention if you experience severe abdominal pain, blood in your stool, or persistent vomiting, as these could indicate a more serious condition that affects your quality of life.


