Key Highlights
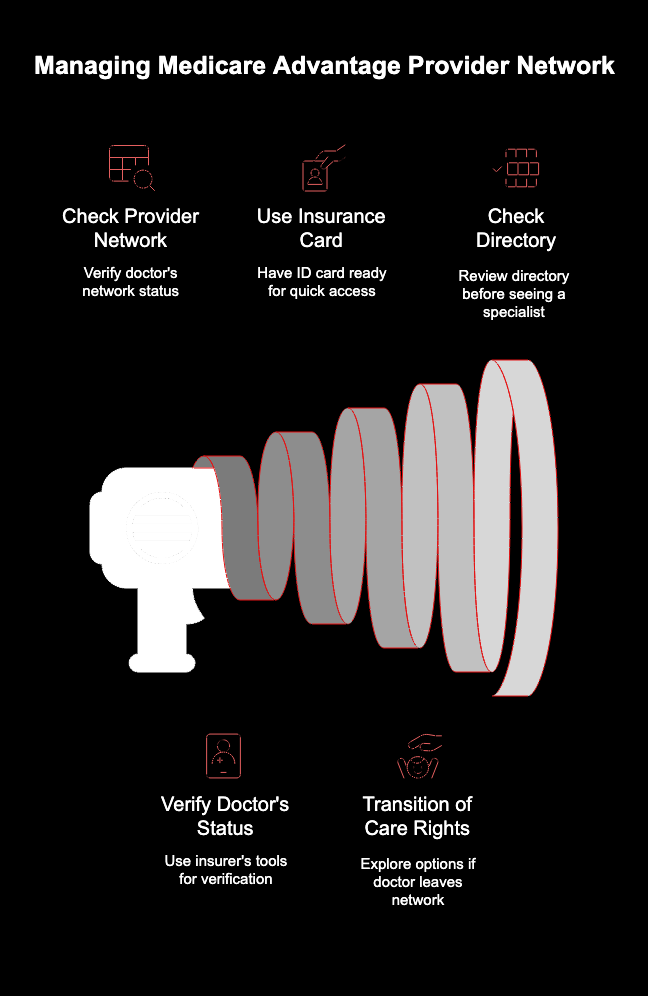
- Your Medicare Advantage plan’s provider network can change, so it’s vital to check it regularly.
- Using an out-of-network health care provider can lead to significantly higher out-of-pocket costs.
- You can quickly verify your doctor’s status using your insurer’s website or mobile app.
- Always have your insurance member ID card handy for the fastest verification.
- If your doctor leaves the network, you may have transition of care rights to continue seeing them temporarily.
- Check your health insurance plan’s directory before seeing a new specialist.
Introduction
If you have a Medicare Advantage plan, you know it offers great benefits. But to make the most of your health plan, you need to ensure your doctors are in your network. Provider networks can change, and seeing a doctor who is no longer in-network can lead to unexpected bills. This guide will show you why it’s so important to confirm your doctor’s status with your insurance company and give you quick, simple ways to do it right now.
Why It’s Essential to Review Your Doctors When You Have Medicare Advantage
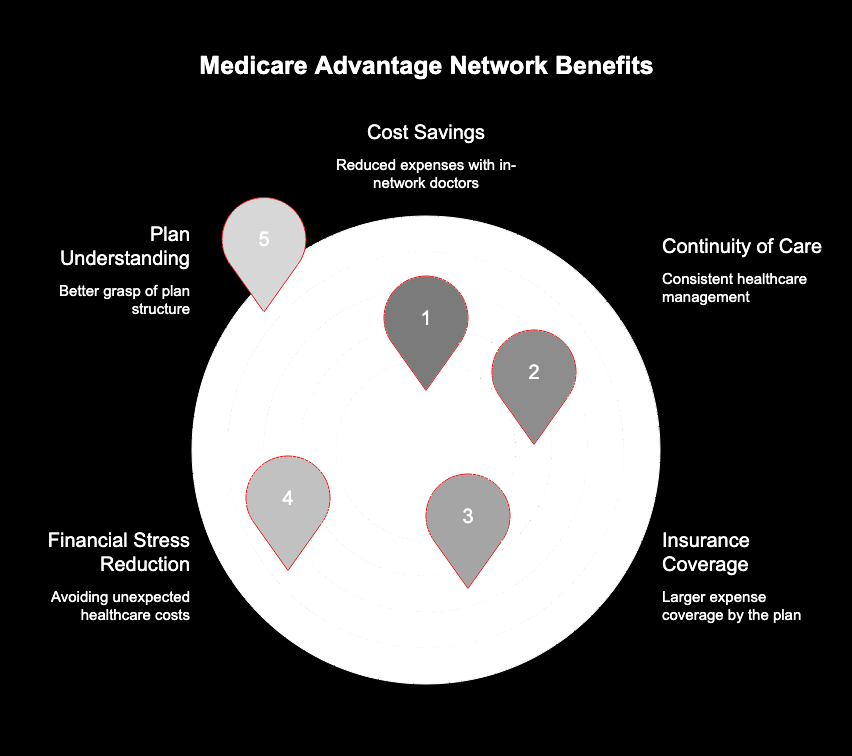
Regularly checking that your doctors are part of your Medicare Advantage plan’s network is crucial for managing your health care costs. Your insurance company negotiates discounted rates with a specific group of doctors. When you see an in-network health care provider, you pay less.
Staying with in-network doctors also ensures continuity of care and helps your health plan cover a larger portion of your expenses. Failing to verify this information can result in you paying much more for services or even the full cost. Taking a few minutes to check can save you from financial stress later. With this knowledge, you can better understand your plan’s structure.
Understanding Your Medicare Advantage Provider Network
What exactly is a provider network? Think of it as a team of doctors, hospitals, clinics, and pharmacies that your health plan has contracted with. Your insurer negotiates with each health care provider to agree on discounted prices for services. This arrangement benefits everyone: you get quality care at a lower price, providers get more patients, and the insurer can manage costs more predictably.
Your Medicare Advantage plan encourages you to use this network. When you stay in-network, your costs are lower, and the payments you make usually count toward your annual deductible and out-of-pocket maximum. The best way to confirm if a provider is in-network is to use the official tools on your insurer’s website or mobile app.
These online portals are the most reliable source of information. They are specifically linked to your health plan and provide the most current details. Simply log in with your member information to access the provider directory and confirm your doctor is covered.
Risks of Not Verifying Your Doctor’s Network Status
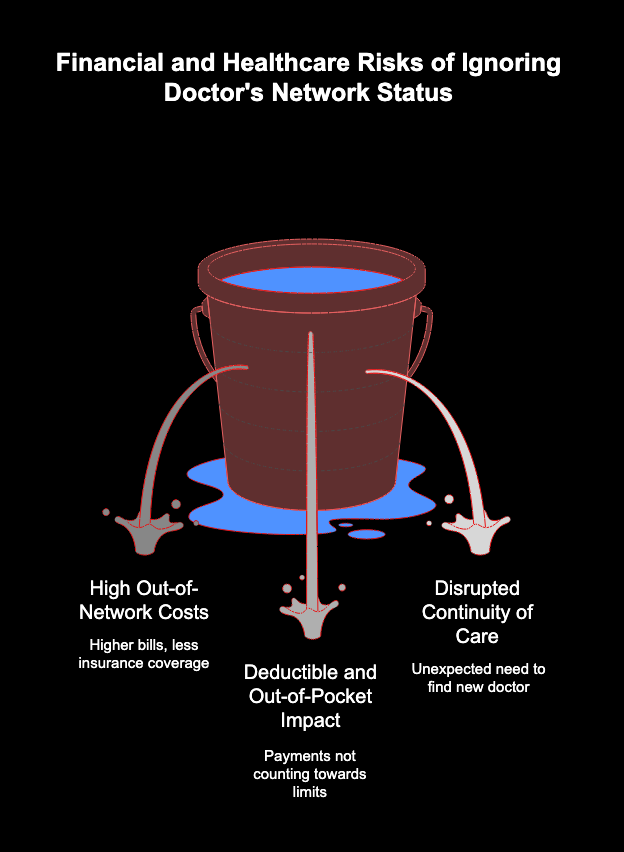
Choosing not to verify your doctor’s network status can expose you to significant financial risks. If you see an out-of-network provider, your insurance company may cover a much smaller portion of the bill, or in some cases, nothing at all. This means you could be responsible for the full cost of your visit, which can be surprisingly high.
Another major risk involves your plan’s cost-sharing features. Payments made for out-of-network services often do not count toward your annual deductible or out-of-pocket maximum. This makes it harder for you to reach these limits, which are designed to protect you from high health care expenses over the year.
Ultimately, neglecting to check the provider network can disrupt your care. You might build a relationship with a doctor based on their knowledge of your health history, only to find out they are not covered. This can force you to find a new doctor unexpectedly, causing stress and a potential gap in your medical care.
Quick Ways to Check if Your Doctor Is In-Network
Worried your doctor might not be covered? Fortunately, there are several fast and easy ways to find out. Your insurance company provides tools designed to give you immediate answers about your network information. The quickest methods are usually online, right at your fingertips.
You can also contact your doctor’s office directly, but it’s crucial to be specific. Ask if they are in your specific plan’s network, not just if they accept your insurance. These simple checks help you avoid unexpected costs and ensure your Medicare Part B and other benefits are applied correctly. The following sections will walk you through exactly how to use these methods for fast results.
Using Official Online Tools for Fast Verification
The fastest and most reliable way to check your doctor’s network status is by using the official online tools provided by your health plan. Nearly every insurer has a member portal on their website and often a mobile app for your smartphone. These resources are directly tied to your plan details and provide up-to-the-minute information.
To get started, you’ll typically need to create an account or log in. Once signed in, you can search for your doctor by name or specialty. The results will clearly indicate whether they are in your network. Using a mobile app is especially convenient, as you can check a provider’s status from anywhere, even while sitting in the doctor’s office waiting room.
Here’s what you’ll need:
- Your insurance member ID card to log in.
- The name and location of the doctor or clinic.
- Access to your insurer’s website or mobile app.
How to Report Directory Inaccuracies
Have you ever found incorrect information in a provider directory? It happens. You might find a doctor listed as accepting new patients when they are not, or their contact information could be outdated. Reporting these inaccuracies helps your insurer keep the directory current, which benefits all members.
If you spot an error, the best first step is to contact your insurer’s customer service department. The phone number is usually on the back of your member ID card. Let them know what information is incorrect and provide the correct details if you have them. You can often submit this information through email or a contact form on the insurer’s website as well.
Reporting an issue is simple and helps improve the service for everyone.
|
Contact Method |
How to Report |
|---|---|
|
Phone Call |
Call the customer service number on your ID card. |
|
|
Send a message to the member services email address. |
|
Online Portal |
Use the “Contact Us” or “Feedback” form on the website. |
Staying Up-to-Date with Network Changes
Provider networks are not set in stone. Your insurer is always evaluating its network to ensure quality and affordability, which means doctors can be added or removed. Because of this, staying informed about your network information is an ongoing responsibility.
Being proactive helps you avoid the surprise of learning your trusted doctor is no longer part of your health plan. It’s wise to make checking your network a regular habit, especially before you need care. The following sections offer guidance on recent updates and how often you should review your provider list to stay ahead of any changes to your Medicare Advantage plan.

Conclusion
In summary, regularly checking your doctors when you have Medicare Advantage is crucial for ensuring you receive the best possible care. Understanding your provider network and the risks associated with not verifying your doctor’s status can save you from unexpected costs and interruptions in your healthcare services. By utilizing online tools and navigating provider directories effectively, you can make informed decisions about your healthcare providers. Remember to stay updated with any network changes and know your rights if your doctor is no longer in-network. For personalized guidance and support, don’t hesitate to reach out for a free consultation today!
Frequently Asked Questions
Does my Medicare Advantage plan notify me if my doctor leaves the network?
While some Medicare Advantage plans may send a letter or email if your primary care physician leaves the network, you shouldn’t rely on it. The best practice is to proactively check your health insurance plan’s provider directory before appointments, as your insurer may not notify you of every change.
Is there a difference between virtual check-ins and regular office visits for coverage?
Often, the cost for a virtual visit is the same as an in-person visit at a doctor’s office, but it depends on your plan. Virtual care providers must still be in-network. Check your plan’s benefits or call customer service to confirm coverage and costs for telehealth services.
Can I check my doctor’s network status in under a minute?
Yes, you absolutely can. Using your insurer’s mobile app or website is the fastest way. Simply log in with your insurance member ID, use the provider network search tool to find your health care provider, and you will get immediate confirmation of their network information.


