Key Highlights
Staying informed about breast cancer screening is a key part of managing your health. The 2025 screening guidelines introduce important updates focused on early detection. Here are the key facts you should know:
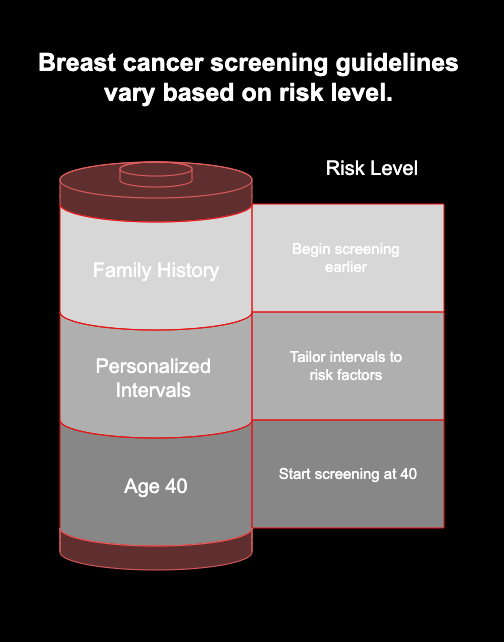
- The recommended age for women at average risk to begin breast cancer screening is now 40.
- Screening intervals are more personalized, based on your individual risk factors.
- Advanced technologies like 3D mammography are now more widely recommended.
- Supplemental tests like breast MRI and ultrasound are integrated for high-risk groups and those with dense breasts.
- Guidelines for those with a family history of breast cancer are more specific, often recommending earlier screening.
Introduction
Navigating the world of breast cancer screening can feel complex, but staying up-to-date is one of the most powerful things you can do for your health. The guidelines for 2025 are shifting toward a more personalized approach, moving away from a one-size-fits-all model. With new research and technology, the focus is on smarter, more effective early detection. Understanding these changes helps you and your provider make the best decisions for your long-term well-being.
Updates in Breast Cancer Screening Guidelines for 2025
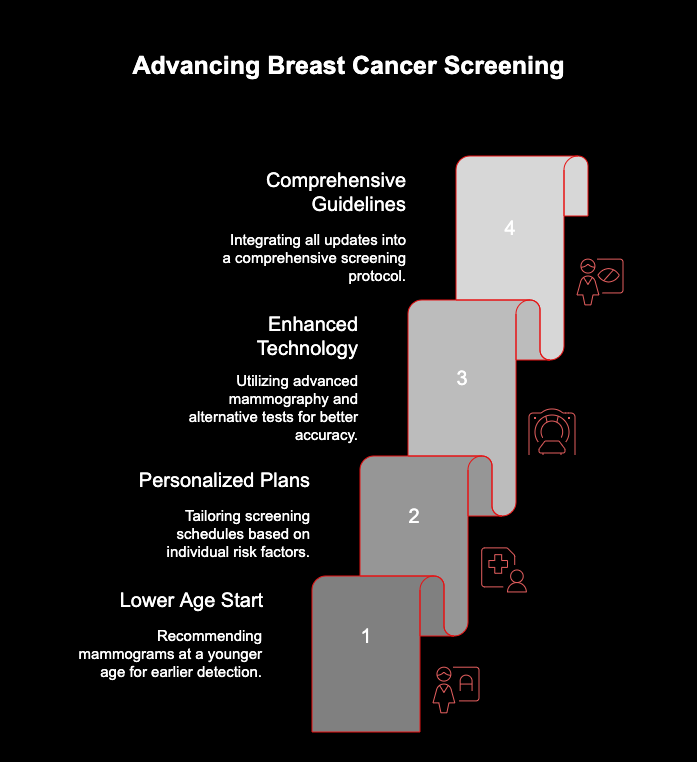
The 2025 breast cancer screening guidelines reflect a significant step forward in proactive health care. A major update is the recommendation to lower the starting age for mammograms, aiming for earlier detection and better outcomes. This change is driven by data showing an increase in breast cancer among younger women.
In addition to age adjustments, the new screening recommendations emphasize a more personalized plan. Your health care provider will consider your unique risk of cancer to determine the right screening schedule for you. The following sections will explore the new age eligibility and recommended screening frequency in more detail.
New Age Recommendations and Eligibility
One of the most notable changes in the 2025 breast cancer screening recommendations is the new starting age. Health organizations like the American Cancer Society now suggest that women at average risk begin yearly mammograms at 40 years of age. This is a shift from the previous recommendation to start at age 45.
This update is a response to studies indicating a rise in breast cancer diagnoses within the 40-44 age group. By starting screening earlier, the goal is to find cancers when they are smaller and easier to treat, potentially reducing the need for more aggressive therapies and improving survival rates.
Your eligibility for screening always depends on a personal risk assessment. It’s crucial to have a conversation with your provider to understand what these new screening recommendations mean for your specific health plan. Every woman’s journey is different, and these guidelines help tailor a path that fits you best.
Screening Frequency: How Often is Recommended?
The 2025 breast cancer screening recommendations also bring updates to how often you should get screened. Instead of a single, rigid timeline for everyone, the guidelines now favor a more flexible approach based on your age and personal risk factors. This ensures that routine screening is optimized for your individual needs.
For women at average risk, the general recommendations for regular mammograms are:
- Ages 40-44: Option to start annual screening with a mammogram.
- Ages 45-54: Annual mammograms are recommended.
- Ages 55 and older: Can switch to a mammogram every other year or continue annually.
Discussing these options with your doctor is essential. They can help you weigh the benefits and create a schedule for cancer screening tests that aligns with your health history and preferences. The goal is to make screening consistent and effective without causing unnecessary testing.
Advances in Breast Cancer Screening Technology
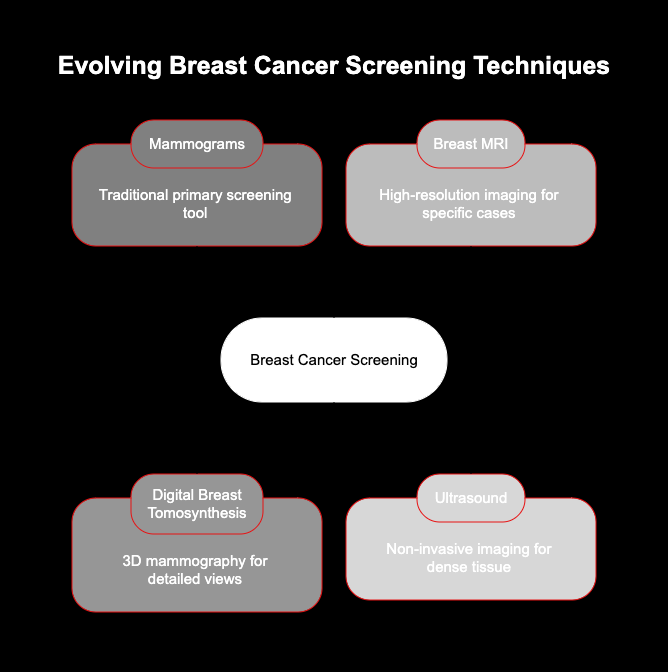
When you think of breast cancer screening, mammograms are likely the first thing that comes to mind. While they remain the primary tool for early detection, the technology behind cancer screening is constantly evolving. In 2025, there is a greater emphasis on using the right test for the right person.
Advanced imaging techniques are becoming more integrated into standard care. Technologies like digital breast tomosynthesis (3D mammography), breast MRI, and ultrasound offer more detailed views and can be particularly helpful for certain individuals. Let’s look at what makes these breast cancer screening tests different.
Enhanced Mammography: What’s Different?
A significant advancement in mammography is digital breast tomosynthesis, also known as 3D mammography. Unlike a traditional 2D screening mammogram that takes a flat image, a 3D mammogram takes multiple pictures of the breast tissue from different angles. These images are then combined to create a clear, three-dimensional picture.
This technology is particularly beneficial for women with dense breast tissue, as it can make it easier to spot abnormalities that might be hidden in a 2D image. The key advantages of 3D mammography include:
- Improved cancer detection rates.
- A lower chance of being called back for follow-up testing.
- Better clarity in viewing breast abnormalities.
Many imaging centers now offer 3D mammography as a standard option. If you have dense breasts or want to explore the most advanced screening available, ask your provider if this enhanced mammogram is right for you.
Alternative and Supplemental Screening Tests
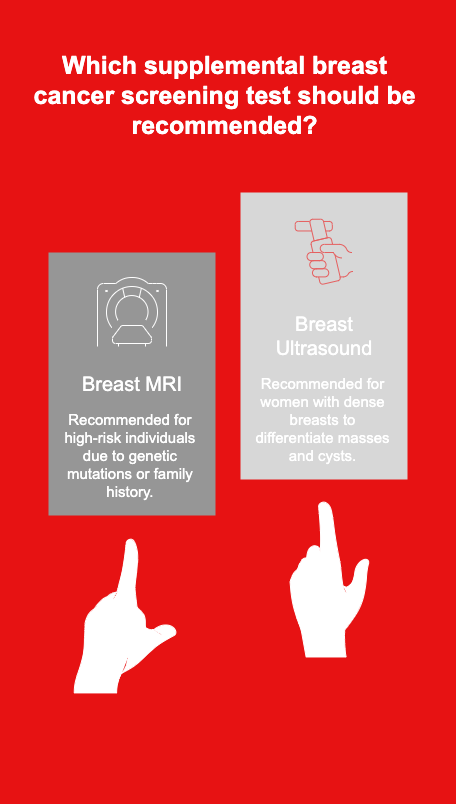
Beyond mammograms, the 2025 guidelines highlight the importance of alternative and supplemental screening tests for certain individuals. A breast MRI, for instance, is a powerful tool for breast cancer detection and is often recommended for those at high risk due to genetic mutations or a strong family history.
Another valuable tool is a breast ultrasound. This test is often used as a supplemental screening method for women with dense breasts, where mammograms may be less effective. It can help differentiate between solid masses and fluid-filled cysts, providing crucial information without using radiation.
It’s important to remember that these tests are typically used in addition to, not as a replacement for, mammograms. Combining different imaging techniques allows for a more comprehensive view of the breast tissue, leading to more accurate diagnoses and better peace of mind.
Family History and Genetic Factors
Having a strong family history of breast cancer is one of the most significant risk factors. The 2025 guidelines provide clear direction for individuals in this situation. A general rule of thumb is to begin screening 10 years earlier than the age your first-degree relative was when they were diagnosed. For example, if your mother was diagnosed at 45, you should start screening at 35.
Risks, Benefits, and Statistics of Breast Cancer Screening in 2025
Making a decision about breast cancer screening involves understanding both the advantages and the potential downsides. The primary benefit of screening is clear: finding cancer early dramatically increases the chances of successful treatment. However, it’s also wise to be aware of the potential harms, such as false positives that lead to extra testing and anxiety.
Understanding the numbers behind breast cancer can also put screening into perspective. Knowing the incidence and survival rates helps highlight why early detection is so crucial. Let’s take a closer look at the benefits versus the risks and what the latest data shows.
Incidence and Survival Rates: What 2025 Data Shows
Statistics for 2025 continue to underscore the importance of screening. Breast cancer remains a leading cancer among women, with over 300,000 new invasive breast cancer cases expected to be diagnosed. While this number is high, the good news is that survival rates are excellent when the disease is found early.
Early detection through regular screening is a major reason for these high survival rates. Different screening tools are recommended based on your personal risk profile to maximize the chances of an early breast cancer diagnosis.
Here is a quick overview of different tests and who they are best for:
|
Screening Test |
Best For |
|---|---|
|
3D Mammography (Tomosynthesis) |
All women, especially those with dense breasts |
|
Breast Ultrasound |
Women with dense breasts or symptoms under 40 |
|
Breast MRI |
High-risk individuals (e.g., with BRCA mutations) |
|
Clinical Breast Exam |
A supplement to imaging for all age groups |
Conclusion
In summary, staying informed about breast cancer screening guidelines and advancements is crucial for everyone. As we approach 2025, it’s essential to understand the new recommendations, particularly for high-risk groups and the latest technologies that enhance screening accuracy. Knowledge empowers individuals to take proactive steps toward their health, ensuring timely interventions when necessary. If you’re uncertain about your screening needs or want personalized advice, don’t hesitate to reach out for a consultation—your health is worth it!
Frequently Asked Questions
What age should you start breast cancer screening in 2025?
According to the 2025 breast cancer screening guidelines, women at average risk should start the conversation about breast cancer screening with their provider at age 40. This update aims to improve early detection for this age group, leading to better treatment outcomes. Your personal risk may require an even earlier start.
How do I prepare for my breast cancer screening appointment?
To prepare for your breast cancer screening, be ready to discuss your personal and family health history with your health care provider. On the day of your breast exam, avoid wearing deodorant, antiperspirant, or lotion, as these can interfere with imaging results. Also, be sure to mention any recent breast changes you’ve noticed.
Are there changes to the American Cancer Society’s recommendations in 2025?
Yes, the American Cancer Society has updated its breast cancer screening recommendations for 2025. One of the key changes is the suggestion for women at average risk to begin screening with a mammogram at age 40. These updates emphasize a more personalized screening plan to enhance early detection and breast cancer awareness.