
Key Highlights
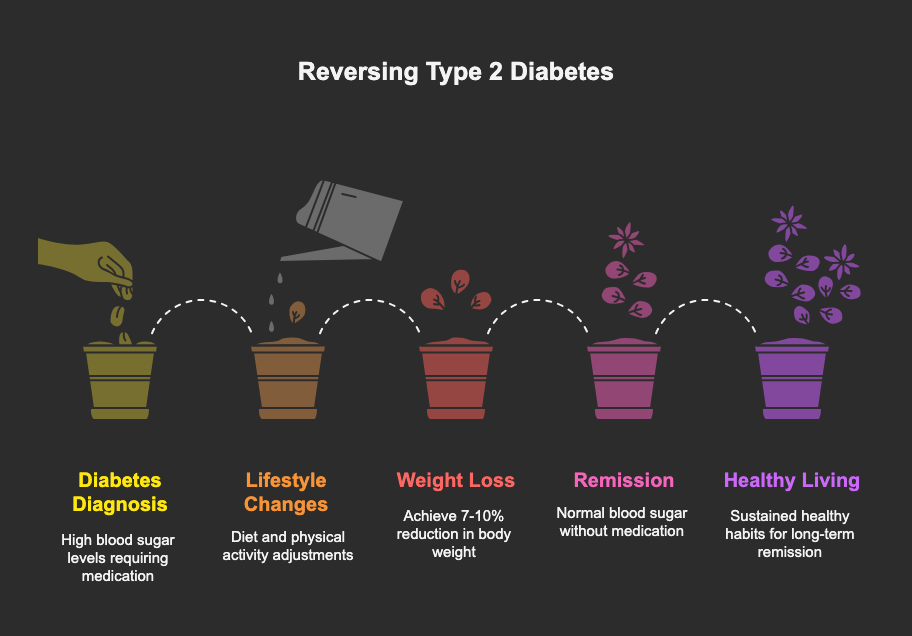
- A diabetes diagnosis isn’t always a life sentence; for many with type 2, remission is an achievable goal.
- Lifestyle changes focusing on diet and physical activity are the cornerstone of reversing prediabetes and managing type 2 diabetes.
- Significant weight loss, even a modest 7-10% of your body weight, can dramatically lower blood sugar and reduce the need for diabetes medication.
- The term “reversal” medically means achieving a state of remission where blood sugar levels are normal without medication.
- While there is no cure, the remission of type 2 diabetes is possible through sustained healthy habits.
Introduction
Receiving a diabetes diagnosis can feel overwhelming, often seeming like a permanent sentence to a chronic disease. You might wonder if this is your new reality forever. But what if it wasn’t? The conversation around diabetes is changing, with more focus on the possibility of reversal. This article will explore what it truly means to reverse diabetes, separating fact from fiction and outlining the proven strategies that can help you regain control of your blood sugar and your health.
Understanding Diabetes: A Brief Overview
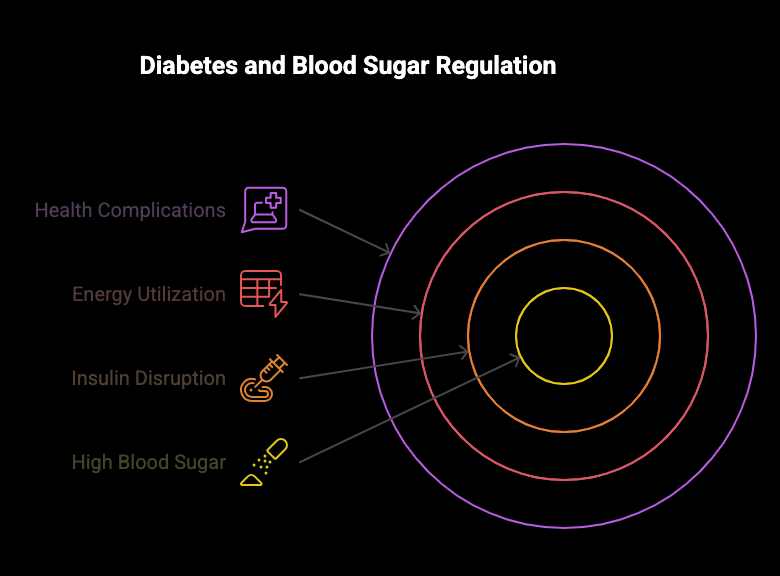
At its core, diabetes is defined by one primary issue: high blood sugar. This happens when your body’s system for regulating glucose, managed by the hormone insulin, goes wrong. Insulin’s job is to help sugar from your bloodstream enter your body’s cells to be used for energy.
When this process is disrupted, glucose builds up in the blood, which can lead to serious health complications over time, like kidney disease and vision loss. Think of it less as an on-off switch and more like a slider. Is it possible for diabetes to go away completely or is it a lifelong condition? While you can’t switch it “off,” positive lifestyle changes can move the slider away from a diabetes diagnosis and toward better disease control.
Key Differences Between Type 1 and Type 2 Diabetes
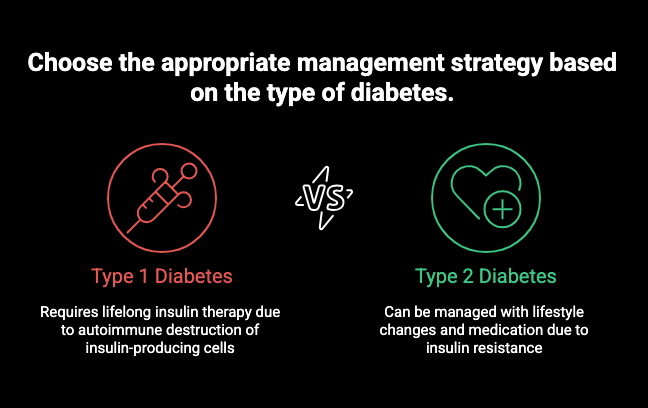
It’s crucial to understand that not all diabetes is the same. The two main types, Type 1 and Type 2, have very different causes and mechanisms. Type 1 diabetes is an autoimmune condition where the body mistakenly attacks its own pancreas, destroying the beta cells that produce insulin. This results in an insulin deficit, meaning people with Type 1 must get insulin from an outside source.
In contrast, Type 2 diabetes, which accounts for about 95% of cases, is characterized by insulin resistance. The body produces insulin, but the cells don’t respond to it properly. This resistance is often driven by excess weight, particularly fat around the stomach. Over time, the pancreas can’t produce enough insulin to overcome this resistance, leading to high blood glucose.
Understanding these differences is key because the concept of “reversal” primarily applies to Type 2 diabetes, which is often linked to lifestyle factors.
|
Feature |
Type 1 Diabetes |
Type 2 Diabetes |
|---|---|---|
|
Cause |
Autoimmune reaction destroying insulin-producing cells. |
Insulin resistance, often linked to genetics and lifestyle. |
|
Insulin Status |
Body produces little to no insulin. |
Body produces insulin, but cells don’t use it effectively. |
|
Onset |
Often develops quickly, typically in childhood or adolescence. |
Develops gradually over months or years, usually in adults. |
|
Primary Management |
Lifelong insulin therapy. |
Lifestyle changes, oral medication, and sometimes insulin. |
What Is Prediabetes and How Does It Progress?
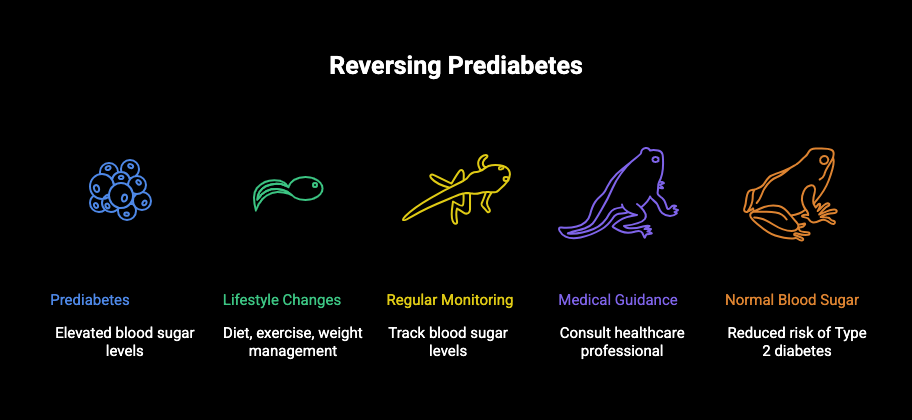
Before a full Type 2 diabetes diagnosis, many people experience a condition called prediabetes. This is a serious warning sign where your blood sugar levels are higher than the normal range but not yet high enough to be classified as diabetes. According to the CDC, one in three American adults has prediabetes, and a staggering 80% don’t even know it.
Without intervention, prediabetes puts you at a much higher risk of developing Type 2 diabetes within five years. It also increases your risk for heart disease and stroke. The progression happens as your body’s insulin resistance gradually worsens, making it harder to keep blood sugar under control.
So, is prediabetes reversible, and how is it different from type 2 diabetes reversal? Absolutely. Prediabetes is highly reversible. By making proactive lifestyle changes, you can often bring your blood sugar levels back down to a normal range and prevent or significantly delay the onset of Type 2 diabetes.
The Role of Genetics and Family History
If diabetes runs in your family, you may worry that it’s an inevitable part of your future. It’s true that genetics and family history create a genetic predisposition for Type 2 diabetes, putting you at a higher risk. If a parent or sibling has the condition, your chances of developing it increase.
However, as UCLA expert Dr. Obidiugwu (Kenrik) Duru states, “genes are not your destiny.” Even with a strong family history, you have the power to influence your health outcome. The lifestyle choices you make every day can significantly lower your risk and help you avoid going down the same path as your relatives.
This genetic component is part of why some experts say diabetes can’t be fully “cured” or “reversed” in the traditional sense; the underlying predisposition remains. Even in remission, the genetic risk factor doesn’t disappear, which is why maintaining a healthy lifestyle is a lifelong commitment.
Lifestyle Factors That Increase Risk
While you can’t change your genes, you can change your lifestyle. Certain habits significantly increase your risk of developing prediabetes and Type 2 diabetes. Excess weight, particularly around the abdomen, is a primary driver of insulin resistance and weight gain is a major risk factor.
A diet high in unhealthy foods also plays a huge role. Over-consuming certain types of foods can contribute to the development of diabetes. You can see how making different choices can help create healthy habits.
Here are some lifestyle factors that raise your risk:
- An Unhealthy Diet: Consuming too many processed foods, sugary drinks, fried foods, and simple carbohydrates like white bread and pastries.
- Lack of Physical Activity: Exercising fewer than three times a week can contribute to weight gain and decreased insulin sensitivity.
- Being Overweight: Carrying excess weight is one of the most significant risk factors for developing Type 2 diabetes.
Can type 2 diabetes be reversed with lifestyle changes? Yes, addressing these very factors is the key to prevention and reversal.
What Does “Reversal” Mean in Medical Terms?
So, what does it mean to “reverse” diabetes medically? The term “reversal,” or more precisely, “remission,” refers to the state where your blood sugar levels return to a non-diabetic range without the help of any diabetes medication. For example, this would mean achieving an A1C level below 6.5% after stopping your medications.
This state of disease control is achieved by addressing the root causes of Type 2 diabetes, primarily insulin resistance. By making significant lifestyle changes, such as losing weight and increasing physical activity, many individuals can restore their body’s ability to manage glucose effectively. The goal is to achieve the remission of type 2 diabetes and maintain it long-term.
It’s not a one-time fix. Achieving remission is a major victory, but maintaining it requires a permanent commitment to the healthy habits that got you there. If you revert to your previous lifestyle, your blood sugar levels will likely rise again.
Proven Strategies for Reversing Type 2 Diabetes
Are there proven methods for reversing type 2 diabetes? Yes, and they are accessible to most people. The most effective strategies revolve around intensive lifestyle management. The primary focus is on achieving significant weight loss through a combination of dietary changes and increased physical activity.
These approaches work by directly targeting insulin resistance, helping your body use glucose more efficiently. The health benefits extend far beyond blood glucose control, improving your overall well-being. The following sections will detail the specific dietary and exercise plans that have proven successful.
Alternative and Advanced Approaches
Beyond traditional diet and exercise, other approaches can help in the journey toward diabetes remission. Some people explore methods like intermittent fasting, while others may be candidates for more significant medical interventions. These advanced strategies can lead to substantial weight loss and improved health outcomes.
For individuals with a higher body mass index, options like bariatric surgery have shown remarkable success in reversing Type 2 diabetes. These methods offer powerful alternatives when lifestyle changes alone aren’t enough. We’ll now look at intermittent fasting and surgical options in more detail.
Intermittent Fasting: Promise and Pitfalls
Can intermittent fasting actually reverse type 2 diabetes? While many fad diets, including various fasting protocols, may help you lose weight, there is limited research on their long-term benefits specifically for diabetes prevention. The most important dietary goal is to lose weight and maintain a healthier body weight for life.
The key to success isn’t necessarily one specific diet but finding an approach you can stick with. Sustainable, positive lifestyle changes are what truly matter. Whether it’s intermittent fasting or another plan, the underlying principle is to consume fewer calories in a way that works for you.
Before trying any new diet, remember:
- The goal is sustainable weight loss, not a temporary fix.
- Healthy dietary choices should become lifelong habits.
- Focus on nutrient-dense foods that support stable blood glucose.
Conclusion
In summary, understanding the complexities of diabetes is essential for anyone navigating this condition. While some experts assert that diabetes is a lifelong challenge, others point to proven strategies that can lead to significant improvements, especially for those with Type 2 diabetes. Adopting healthier lifestyle choices, such as dietary changes and increased physical activity, can make a difference in managing or even reversing the condition. Additionally, exploring advanced approaches may open new avenues for those seeking better health outcomes. If you’re ready to take control of your health journey and explore your options further, we invite you to get a free consultation with our specialists. Your path to better health starts here!
Frequently Asked Questions
How long does it take to see results from diabetes reversal strategies?
Results from lifestyle changes can appear relatively quickly. You might notice improvements in your blood sugar levels within a few weeks of consistent effort. Meaningful weight loss often occurs at a pace of 1-2 pounds per week, with significant health benefits and potential for remission becoming apparent over several months of sustained commitment.
Are there risks to trying to reverse diabetes?
Yes, it’s crucial to work with a healthcare provider. Making drastic changes to your diet or exercise, especially if you are on diabetes medication, can cause your blood glucose to drop too low. Professional guidance ensures proper disease control and helps you avoid potential health complications while safely working toward remission.
Is prediabetes truly reversible or just manageable?
Prediabetes is truly reversible. Experts from institutions like the Yale School of Medicine confirm that proactive lifestyle modifications can bring your blood sugar back down into the normal range. This effectively reverses the condition and can prevent or significantly delay the onset of Type 2 diabetes, offering a critical window for action.


