
Key Highlights
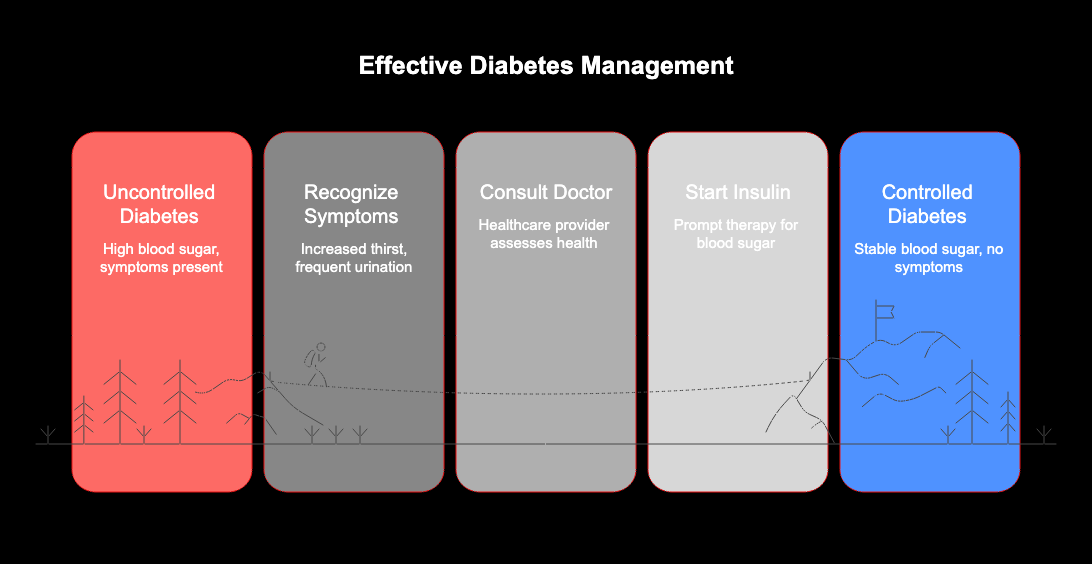
- Starting insulin therapy promptly is a key part of effective diabetes management when other treatments are not enough.
- Persistently high blood sugar is a primary indicator that you may need immediate insulin.
- Pay attention to symptoms of uncontrolled diabetes, such as increased thirst, frequent urination, and blurred vision.
- A healthcare provider determines the need for insulin based on your health status and how well other medications are working.
- Delaying recommended insulin treatment can lead to serious short-term and long-term health complications.
Introduction
Navigating diabetes management can bring up many questions, and one of the most significant is about starting insulin therapy. While oral medications and lifestyle changes are often the first line of defense, there are times when your body needs more help to control blood sugar. Knowing when to start insulin right away is crucial for your long-term health. Are you aware of the signs that signal your diabetes management plan needs to change? Let’s explore the key indicators that it’s time to talk to your doctor about insulin.
Understanding Insulin Therapy in Diabetes Management
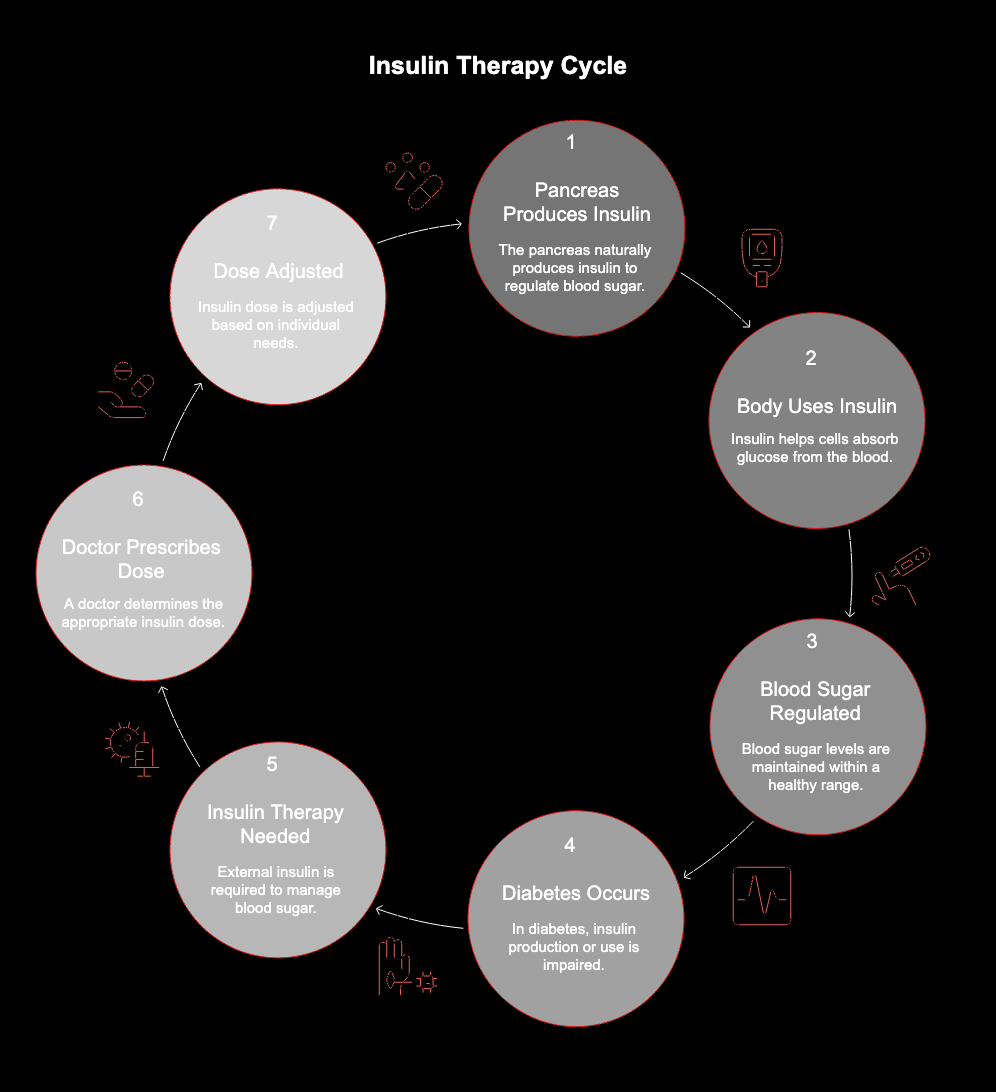
Insulin therapy is a cornerstone of diabetes management for many people, helping to keep blood glucose levels in a healthy range. When your body can’t produce enough insulin on its own, prescribed insulin steps in to do the job, preventing the complications of high blood sugar.
There are different types of insulin designed to work in various ways. Understanding what insulin is and the main differences between them can help you feel more confident in your treatment plan.
What Is Insulin and Why Is It Needed for Diabetes?
Insulin is a hormone that your pancreas would normally produce to help regulate blood sugar. In people with diabetes, the body either doesn’t make enough insulin or can’t use it effectively. This is why insulin treatment becomes necessary. For individuals with type 1 diabetes, insulin therapy is essential for their whole life.
For those with type 2 diabetes, insulin is recommended when other treatments, like oral medications, are no longer sufficient to manage blood glucose. The goal is to provide the right amount of insulin to keep you healthy and prevent the symptoms of high blood sugar.
Working with your doctor helps ensure you get the correct insulin dose for your specific needs, which can change based on factors like illness, stress, or activity levels.
Differences Between Long-Acting and Short-Acting Insulin
When you begin insulin treatment, your healthcare provider will prescribe one or more types of insulin. The two main categories are long-acting and short-acting insulin, and they serve different purposes in managing your blood sugar throughout the day.
Long-acting insulin provides a steady, background level of insulin to keep your blood glucose stable between meals and overnight. In contrast, short-acting insulin is taken before meals to manage the spike in blood sugar that occurs after you eat. Your required insulin dose for each type will depend on your weight, activity, and diet.
Here’s a simple breakdown of their differences:
|
Feature |
Long-Acting Insulin |
Short-Acting Insulin |
|---|---|---|
|
When to Take |
Once or twice a day, at the same time each day. |
Around 30 minutes before each meal. |
|
Primary Goal |
Provides a consistent baseline of insulin. |
Manages blood sugar spikes from meals. |
|
Dose Calculation |
Usually a set dose prescribed by your doctor. |
Dose is often adjusted based on carbohydrate intake. |
Key Signs That You Need to Start Insulin Right Away
Recognizing the key signs that your body needs insulin is vital. If your current diabetes plan isn’t keeping your blood sugar levels under control, your body will start showing symptoms of high blood glucose. These signals are your body’s way of telling you that it’s time for a more effective treatment.
Listening to your body and monitoring these changes can help you and your doctor decide on the next steps. Let’s look at some of the most important signs that you may need to start insulin immediately.
Rapidly Rising Blood Sugar Levels
One of the most direct signs is consistently high blood glucose readings that don’t come down with your current treatment. If you are tracking your blood sugar and notice it is frequently elevated, it’s a clear warning. This indicates that your body is struggling to manage glucose on its own.
The risk of high blood sugar increases when your body has too little insulin. You may notice this after eating certain foods, particularly high sugar snacks, but persistent elevation is the main concern.
Symptoms that often accompany rapidly rising blood sugar include:
- Feeling very thirsty
- Needing to urinate more often than usual
- Constant tiredness or fatigue
- Blurred vision
If you experience these, it’s important to speak with your healthcare team.
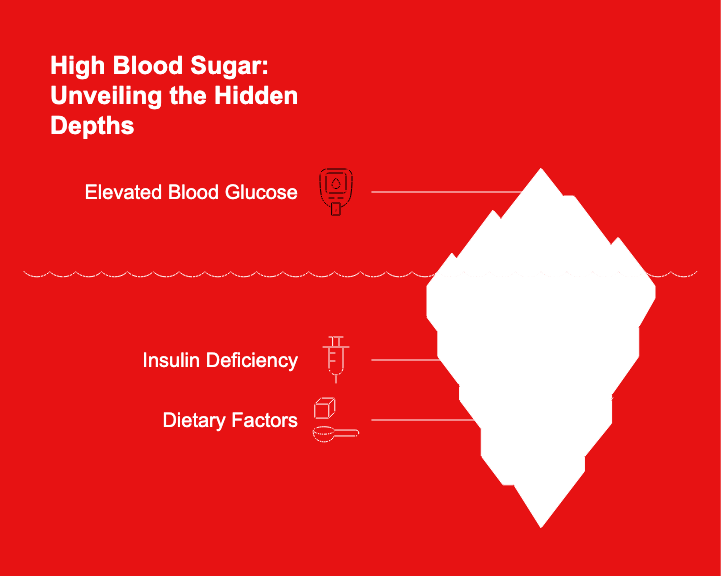
High A1C Readings and Immediate Risks
Your doctor uses tests like the A1C to get an average picture of your blood sugar control over several months. A high A1C reading confirms that your blood sugar has been consistently elevated, putting you at immediate risk for complications. This is a strong clinical indicator that a change in treatment, such as starting regular insulin, may be necessary.
High readings point to a failure to maintain control and signal that your body needs more support. The immediate risks associated with unchecked high blood sugar are serious and require prompt medical attention.
These risks include:
- Severe hyperglycemia, which can damage your body.
- An increased chance of developing long-term complications affecting your heart, nerves, and kidneys.
Clinical Criteria for Starting Insulin
Doctors follow clear clinical criteria when recommending insulin. The primary factor is whether your blood glucose levels are consistently high despite being on other diabetes medications. If your blood sugar remains elevated, it’s a sign that your body requires insulin to achieve control.
Your type of diabetes is also a major consideration. For people with type 1 diabetes, insulin is a lifelong necessity from diagnosis. For those with type 2 diabetes, it’s typically introduced when oral medications and lifestyle adjustments are no longer enough to manage high blood sugar.
The ultimate goal is to find the right dose of insulin to bring your levels into a healthy range and prevent the negative effects of hyperglycemia. Your healthcare team will work with you to tailor a plan that fits your specific situation.
What Happens if Insulin Is Delayed When Recommended
Delaying the start of insulin therapy when your doctor recommends it can have significant consequences for your health. When your body isn’t getting the right amount of insulin it needs, your blood sugar will remain high. This state of prolonged high blood sugar, or hyperglycemia, is harmful to your body.
Postponing delayed insulin treatment means you miss out on the chance to get your blood glucose under control, which is the most important step in preventing both immediate symptoms and long-term diabetic complications. Ignoring the recommendation can lead to a preventable decline in your health. Let’s look at the specific effects.
Impact on Diabetes Complications
The most critical reason not to delay insulin is its impact on diabetes complications. When blood glucose levels are not managed, the risk of developing these complications increases dramatically. This is not a risk worth taking.
Uncontrolled blood sugar can lead to severe hyperglycaemia. In the worst cases, it can cause a life-threatening condition called diabetic ketoacidosis. These are serious, acute problems that require emergency medical care.
The long-term effects are just as concerning. Chronic high blood sugar can cause irreversible damage to your:
- Heart and blood vessels
- Kidneys
- Eyes, potentially leading to blindness
- Nerves, especially in your feet
Starting insulin when recommended is a powerful tool to prevent these devastating complications.
Conclusion
Recognizing the key signs that indicate a need for immediate insulin therapy is crucial in managing diabetes effectively. By understanding the symptoms of uncontrolled diabetes and the implications of delayed treatment, you empower yourself or your loved ones to take swift action when necessary. Timely intervention not only helps regulate blood sugar levels but also prevents potential short-term and long-term complications associated with diabetes. Remember, your health is a priority, and being proactive about insulin therapy can significantly enhance your quality of life. If you have any concerns about your diabetes management, don’t hesitate to consult with your healthcare provider for personalized guidance.
Frequently Asked Questions
Should people with type 2 diabetes start insulin sooner rather than later?
For people with type 2 diabetes, starting insulin treatment is recommended when other medications fail to control blood sugar. Beginning insulin therapy sooner when needed can help you get the right dose to prevent long-term complications, so it is often better not to delay injections if your doctor advises them.
What are the first steps when beginning insulin therapy for diabetes?
When you begin insulin therapy, a diabetes nurse will guide you through the first steps. They will show you how to perform a daily insulin injection, how to use your pen or pump, and the importance of rotating the injection site to keep your skin healthy and ensure proper insulin absorption.
Are there specific blood sugar levels that mean insulin should be started immediately?
While there isn’t a single magic number, consistently high blood sugar levels that do not respond to other treatments are a key sign. Your health care provider or diabetes specialist will evaluate your readings and symptoms to determine if immediate insulin is the right step for your health.


